For Those Who Have Difficulty Raising Their Shoulder
- Rotator Cuff Tear Arthropathy
- Reverse Total Shoulder Replacement Surgery (Reverse Shoulder Arthroplasty)
If You Have the Following Symptoms, You May Have Rotator Cuff Tear Arthropathy
【Symptoms】
- Limited shoulder movement with grinding noises.
- Minimal pain when the shoulder is not moved, but intense pain upon movement.
- Unable to raise the arm above shoulder height (indicative of severe deformation). The shoulder cannot be raised to the side.
If you have these symptoms, it is possible that the shoulder bone is deformed as shown in the illustration. The diagram below shows a normal shoulder on the left and a deformed shoulder joint (rotator cuff tear arthropathy) on the right.
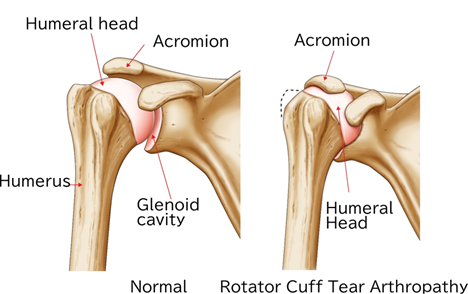
Differences in the Illustrations
Although not shown in the illustration, the difference between a normal shoulder and one affected by rotator cuff tear arthropathy is that the rotator cuff (the tendons of the inner muscles) covering the humeral head is significantly torn, causing the humeral head to come into contact with the acromion.
【Treatment plan】
【For Those Who Do Not Move Their Shoulder Much and Only Wish to Alleviate Pain】
In cases where the main goal is to alleviate pain and the shoulder is not moved much, the first choice of treatment is usually conservative therapy. This often involves injecting medication into the joint to reduce inflammation, combined with rest, which frequently alleviates shoulder pain.
【If the Pain Has Subsided】
When shoulder pain has subsided, exercise therapy is recommended. Even in the state of rotator cuff tear arthropathy, it is often possible to raise the arm. Why is it possible to raise the arm even with a torn rotator cuff? This is still not clearly understood. Additionally, in rotator cuff tear arthropathy, the glenoid cavity of the scapula (refer to the section on total shoulder replacement surgery) is often damaged. The extent of bone deformation varies from person to person. Therefore, exercise therapy may be effective for some individuals and not for others.
【If Conservative Therapy (Non-surgical Treatment) is Ineffective】
Several surgical treatments are recommended:
- Arthroscopic Synovectomy
Using an endoscope to observe the joint, degenerated (non-normal) tissues of the rotator cuff and synovium are cleaned. While pain relief is achieved, the extent of movement improvement varies from person to person. - Humeral Head Replacement Surgery
This surgery replaces only the humeral head with an artificial head. Unlike total shoulder replacement surgery, humeral head replacement does not address the glenoid cavity. Improvement in the range of motion can be expected for those who can raise their shoulder despite pain. However, for those who have shoulder pain and cannot raise their arm, the improvement in symptoms is less likely with humeral head replacement. Therefore, the indication for humeral head replacement in rotator cuff tear arthropathy is determined by the physician based on the symptoms and the patient's functional recovery goals.
【New Treatment Methods for Those Who Have Difficulty Raising Their Shoulder】
There are reports that reverse shoulder arthroplasty, approved for use domestically since April 2014, is effective. This reverse shoulder arthroplasty has been used in Europe since the 1990s and in the United States since 2004.
【Reverse Shoulder Arthroplasty (Reverse Total Shoulder Replacement) 】
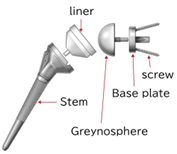
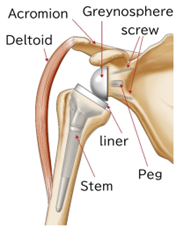
Reverse shoulder arthroplasty (reverse total shoulder replacement) involves inserting instruments, as shown in the illustration, into the scapula and humerus of the shoulder. In the illustration below, a plastic liner and stem are inserted into the deformed humerus, while a metal ball (glenosphere) and baseplate are placed into the glenoid cavity of the scapula. The baseplate is fixed with metal screws.
The diagram below shows the reverse shoulder prosthesis inserted into the humerus and scapula. The stem and liner are connected.
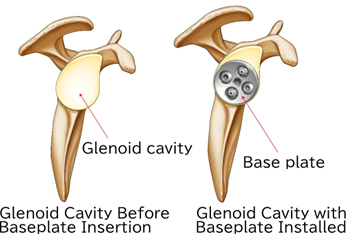
The diagram below shows the baseplate inserted into the glenoid cavity of the scapula.
Why It is Called Reverse Shoulder Arthroplasty (Reverse Total Shoulder Replacement)
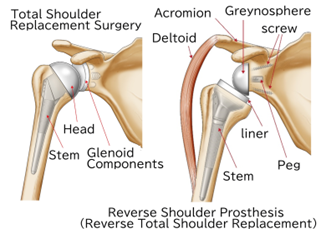
In total shoulder replacement surgery, the damaged humeral head is replaced with a head, and the damaged glenoid cavity is fitted with a glenoid component. This surgery is performed when the rotator cuff (tendons of the inner muscles) is not damaged (refer to the section on total shoulder replacement surgery). Therefore, the shoulder's structure resembles the original shoulder anatomy. However, in reverse shoulder arthroplasty, the glenosphere, which is the equivalent of the round head, is placed in the glenoid cavity, and the liner for the glenosphere is placed on the humeral side. Unlike total shoulder replacement surgery, the head and liner are in opposite positions. Hence, it is called reverse shoulder arthroplasty (reverse total shoulder replacement).
【X-rays Before and After Reverse Shoulder Arthroplasty (Reverse Total Shoulder Replacement) 】
Normal X-ray
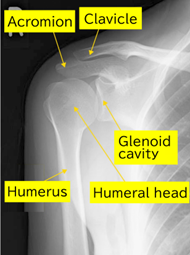
X-ray Before Surgery (X-ray of Rotator Cuff Tear Arthropathy)

Refer to the Illustration of Rotator Cuff Tear Arthropathy. The Space Between the Humeral Head and Acromion is Absent Compared to Normal.
X-ray After Surgery
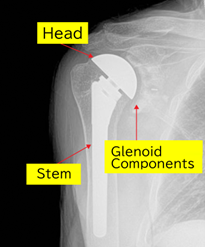
The deformed humeral head is removed, and a plastic liner is also placed in the scapula.
The deformed humeral head is removed, and a plastic liner is also placed in the scapula.
Rehabilitation varies between facilities, but generally, patients wear a brace for several weeks. Gradual rehabilitation follows. Based on my experience observing clinical settings in the United States, some patients can raise their arms to head height within three months. However, the timing and extent of improved range of motion vary greatly between individuals. Therefore, it is recommended to consult with your primary physician.
【Shoulder Movement After Rehabilitation】
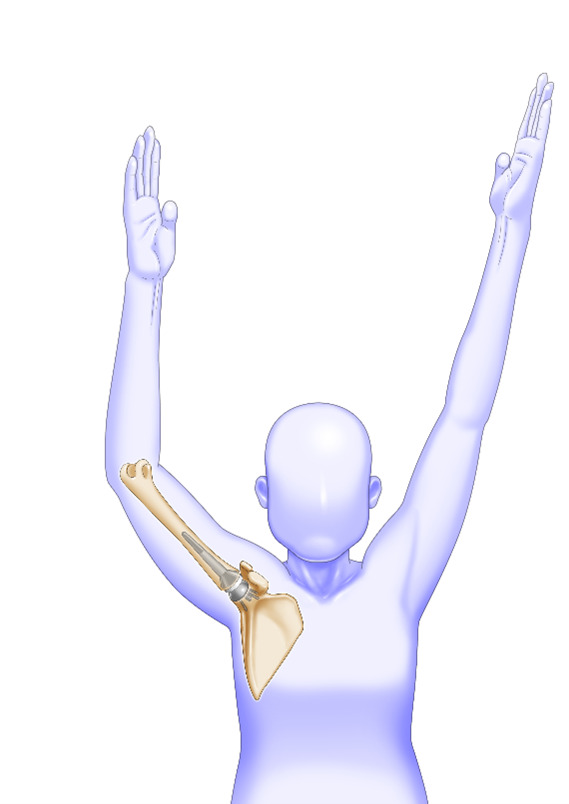
The illustration shows the average way the shoulder moves. Please understand that it is difficult for it to be exactly the same as the healthy side.
【Recovery Guidelines After Reverse Shoulder Arthroplasty (Reverse Total Shoulder Replacement) 】
- Shoulder Elevation: The shoulder may become able to be raised. In some cases, as shown in the photo, this can happen as early as three months post-surgery. However, it may take longer for smaller women due to weaker deltoid muscle strength.
- External Rotation: Generally, external rotation is not significantly improved. However, if the arm could be externally rotated before surgery, it is often possible to maintain or slightly improve this range post-surgery. Individual differences exist.
- Internal Rotation (Reaching Behind the Back): Achieving internal rotation is challenging post-surgery. Activities such as reaching behind the back, fastening a bra, or wiping after using the toilet may be difficult. The degree of internal rotation achieved varies among individuals.
- Re-replacement Surgery Cases: For individuals who have already undergone some type of surgery, the range of motion improvement may be less than that achieved after the initial reverse shoulder arthroplasty.
In the past, the prognosis for total shoulder replacement surgery was not considered very good. This was because the plastic liner mentioned above would loosen within a few years, meaning it would shift or detach from the scapula, causing pain to recur. However, with recent medical advancements, it is expected that the plastic liner may not loosen for about ten years. This expectation is based on reports from facilities worldwide (such as in the United States and France) where total shoulder replacements are commonly performed. Therefore, it is recommended to discuss with your primary physician how long the shoulder prosthesis is expected to last.
Regarding activities such as sports and how much weight can be lifted, there is no unified opinion yet. My mentor, Dr. Williams, advised patients not to lift more than 10kg with both hands. Some patients who underwent total shoulder replacement surgery under Dr. Williams even played golf. However, the ability to participate in sports like golf varies depending on the patient's muscle strength and other factors. Therefore, it is recommended to consult with your primary physician regarding activities and the amount of weight you can lift.
【Specific Complications After Reverse Shoulder Arthroplasty】
We will discuss the representative examples of complications that can occur during or after reverse shoulder arthroplasty. The probabilities of complications have been reported from facilities worldwide and vary widely, so specific figures are not included here. As clinical data in Japan is not yet complete, it is recommended to consult with your primary physician.
- Infection and Suppuration"
The artificial joint is a foreign object to the human body. Infection can occur early after surgery, or even if the course is favorable, bacteria may invade around the artificial joint when the body's immune system is weakened, causing suppuration. Symptoms such as shoulder swelling, persistent fever, or sudden severe pain may indicate an infection. During surgery, doctors use antibiotics via IV and wash the area to prevent bacteria from settling. However, infection is a complication that can occur postoperatively. The frequency of infection varies between facilities, so specific figures are not mentioned here. For reference, at Thomas Jefferson University, where I studied abroad, the infection rate was communicated to patients as 4% for initial surgeries. - Nerve Damage
In reverse shoulder arthroplasty, muscles must be moved, and ligaments of the joint must be excised to place the instruments accurately. These maneuvers may cause transient nerve damage (numbness in the hand, difficulty bending the elbow for a few days) due to arm traction. - Scapular Notch
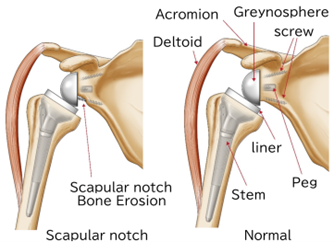
Due to the shape of the reverse shoulder prosthesis implant, the action of touching the opposite shoulder with the arm is more restricted compared to normal. When the liner and scapula bone come into contact during this action (called shoulder adduction and internal rotation), repeated contact can cause the scapula bone to erode, which is referred to as scapular notching. Symptoms include sounds during shoulder adduction and internal rotation. It is said that this does not cause severe pain. However, the liner wears down, and X-rays show erosion of the scapula bone. Currently, there is no established method to treat scapular notching once it occurs, i.e., the erosion of the bone. Therefore, it is essential to take great care in placing the glenosphere to prevent scapular notching. Sometimes the size of the glenosphere is adjusted to address this issue. The frequency of scapular notching varies between facilities, so it is recommended to discuss this with your primary physician before undergoing surgery. - Acromial Fracture
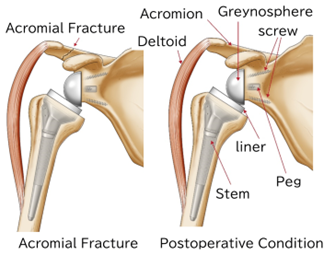
A fracture of the acromion may occur after surgery. The length of the upper limb may become slightly longer. The humerus is supported by the deltoid muscle, but if the upper limb becomes too long, it is thought that the deltoid muscle pulls on the acromion, causing it to fracture.
【Measures for Complications After Total Shoulder Replacement Surgery】
- Infection: Depending on the extent, reoperation may be necessary. In cases of infection, antibiotics are administered via IV, and the body is washed during surgery to prevent infection. However, there are instances where the infection persists. In severe cases, the artificial joint may need to be removed entirely. If the artificial joint loosens, reoperation may also be required. A representative case is when the plastic liner in the glenoid cavity (the scapula's socket) causes bone loss. During reoperation, it is very challenging to replace the plastic liner again. Often, only the metal ball and rod in the humerus are replaced. Reoperation is a very complex procedure and should be discussed with your primary physician.
- Scapular Notch: As previously mentioned, there is no established treatment for scapular notching once it occurs. Therefore, preventive measures are taken to avoid scapular notching. Specifically, careful attention is given to the placement of the glenosphere, and sometimes the size of the glenosphere is adjusted. However, this does not always prevent scapular notching.
- Acromial Fracture: For an acromial fracture that unfortunately occurs, conservative treatment such as bracing can help reduce shoulder pain. It is said that shoulder range of motion improves once the fracture heals. However, there are individual differences, and in some cases, range of motion may not fully improve after the fracture. If this happens, please consult with your primary physician.
【Summary of Rotator Cuff Tear Arthropathy】
- Reverse shoulder prosthesis (reverse total shoulder replacement) is effective for rotator cuff tear arthropathy, where the shoulder cannot be raised.
- Since several complications can occur, it is recommended to thoroughly consult with your primary physician when deciding on surgery.
Outpatient Reception & Consultation Hours
| Business Hours | 月 | 火 | 水 | 木 | 金 | 土 | 日 |
|---|---|---|---|---|---|---|---|
| 13:00~17:00 | ● | ● | ー | ● | ● | ー | ● |
| 18:00~20:00 | ● | ● | ー | ● | ● | ー | ● |
【Closed Days】 Wednesday, Saturday, and Public Holidays.
※translates to "Reception ends 30 minutes before the end of consultation hours."
